OVERVIEW
Urban adolescents in India face significant barriers to accessing reliable Sexual and Reproductive Health (SRH) education and preventive services.
Socio-cultural stigma, inadequate school curricula, misinformation online, and discomfort around discussing sexuality limit their ability to understand their bodies and seek timely care. Parents want to support their children but lack the tools and confidence to begin sensitive conversations.
These individual challenges are compounded by systemic gaps. India’s healthcare ecosystem remains fragmented, with inconsistent access to preventive SRH services such as HPV vaccination, early screenings for Cancers, and adolescent-friendly healthcare services (AFHS), particularly for the “Missing Middle,” who fall outside public insurance schemes and depend heavily on private care.
Potli of Care responds to these layered barriers through a culturally grounded, user-centred intervention designed for adolescents aged 10–22 and their caregivers.
The project aims to build early preventive behaviours and long-term SRH autonomy by,
-
Strengthening trusted knowledge
-
Enabling parent-child dialogue at home
-
Improving access pathways through paediatric and gynaecology touchpoints
CONTEXT
A shifting landscape
India’s healthcare system is divided across public and private providers, with no unified source of credible SRH information comparable to the NHS.
Preventive services remain unevenly available, particularly for the “Missing Middle”, a large and growing middle-income segment excluded from public subsidies yet burdened by high out-of-pocket expenses in the private sector, hence making it crucial for them to take preventive healthcare measures.
Low government investment, limited integration between paediatric and gynaecology pathways, and poor continuity of preventive education further constrain access.
Amid this shifting landscape, where national commitments to Universal Health Coverage emphasise promotive and preventive care, there remains a critical gap: culturally relevant, trustworthy SRH guidance that supports early health autonomy and sustained preventive behaviours across adolescence.
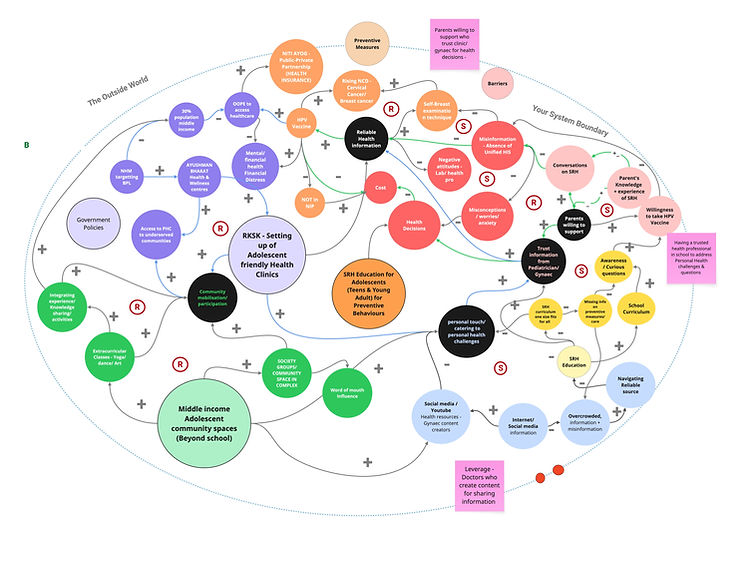
Fig: System map to break down the complexity of the healthcare system in India, key actors, and relationships within the system to identify opportunities
Key contextual challenges:
Systemic barriers
-
A fragmented healthcare system with no unified SRH information source like the NHS in the UK
-
A growing population of middle-income families reliant on private care face high out-of-pocket costs and little structured support.
-
Limited integration between paediatricians and gynaecologists
Individual barriers
-
Stigma and discomfort around adolescent SRH discussions
-
Parents lack tools which are credible, culturally relevant and age-appropriate
-
Adolescents lack autonomy and trusted channels for preventive care
PROBLEM FRAMING

Fig: User scenario to understand a young woman's frustrations and preventive healthcare experience in a Tier 1 city in India
Kajal’s experience uncovers a crucial gap - even young adults who can afford preventive care like HPV, Screenings, Smear tests end up missing it due to individual barriers like negative attitudes from medical professionals, stigma and lack of awareness, but more importantly due to a lack of autonomy.

INSIGHT
Instilling this sense of autonomy, health-seeking & decision-making behavioural change must start at an early stage of Adolescence (10-14) because many health-related behaviours are acquired by individuals during early adolescence, which continue to their adult lives.
(Erik Erikson’s Stages of Psychosocial Development & WHO)

Fig: User scenario to understand how adolescents navigate their puberty
and reproductive healthcare
Urban early adolescents (10–14) and their parents lack a credible, culturally anchored way to:
-
Understand SRH early
-
Build autonomy and preventive behaviours
-
Access adolescent-friendly care
-
Navigate stigma and misinformation
As a result, preventive behaviours are underdeveloped due to a lack of open dialogue, trusted resources, and taboos around gynaecological care, leading to compromised decision-making and autonomy in healthcare.
I believe strengthening early preventive behaviours in adolescents through a credible and culturally-tailored toolkit that enables open SRH dialogue and eases access to gynaecological care will result in stronger autonomy as adolescents grow into adulthood because early exposure to trusted knowledge builds confidence and encourages informed health decisions.
Hypothesis
APPROACH
.png)
A mixed methodology using qualitative, visual, and participatory design tools
5
Structured referral pathways can normalise and build early SRH access
Opportunity
Integrating referral pathways would help adolescents feel more at ease accessing gynaecological care when introduced gradually via trusted doctors, like their paediatrician.
Rewards help sustain engagement
Opportuniy
-
Develop scenario-based gamification tools to spark reflection and understand the child's thinking.
-
Preventive health journey checklist that integrates SRH checklists, puberty milestones, vaccine reminders.
4
RESEARCH INSIGHTS
Strong foundations exists for open dialogue, but parents need support on specific sensitive topics
Opportuniy
Develop conversation tools ( eg, cards, co-learning tools) to support parents in initiating open dialogue on tough conversations without fear or shame.
Parents trust Doctors, not the internet, tools must be medically verified
Opportunity
Ensure the toolkit is distributed/endorsed by experts (e.g., paediatricians/ gynaecologists) to build trust and credibility.
Culturally-tailored, tangible tools may lower barriers and feel trustworthy and personal
(Printed books preferred over the internet)
Opportunity
Using visual storytelling formats to give credible knowledge and normalise access to prevent care services and learn about topics like puberty, vaccination, and hygiene.
1
2
3
How might we build trusted SRH knowledge and enable open dialogue to strengthen early preventive behaviours and informed decision-making to further support health autonomy?
STRATEGY
3 Pillars based on the insights:
Life-course
intervention
A life-stage SRH intervention embedded within existing healthcare touchpoints and a service that supports every teen's SRH journey, every step of the way, one potli at a time
Tangible
toolkit
A physical touchpoint that feels personal and trustworthy, handed over by an expert, builds credibility
Access
Pathways
A referral pathway to bypass systemic and socio-cultural barriers
OUTCOME
Introducing
Potli of Care
A physical toolkit distributed through paediatric clinics, encouraging parents and adolescents to learn together through culturally familiar tools to:
-
Increase adolescents’ SRH knowledge
-
Reduce shame and stigma
-
Strengthen their confidence in accessing SRH services

What's in the Potli?
1
Informative Zine Collection
-
Step-by-step guides (e.g., Self-Breast Exam, HPV vaccine importance)
-
Doctor-reviewed, literacy-friendly content to support curiosity and confidence
2
Loopin Scenario Cards (‘What Would You Do If…’)
-
Challenge stigma through culturally-tailored scenarios that enable reflective discussions
3
Preventive SRH Care Checklist
-
Take ownership of your health, keep a track of vaccines, immunisations and crucial tests to avoid future health risks
4
Stickers, Badges and Rewards
-
Reward-based system (stickers, badges) to sustain engagement
%20copy.png)
How might we ease access to gynaecological care to strengthen early preventive behaviours and informed decision-making to further support health autonomy?



How does it integrate into Jiya's life?
%20copy%202.png)
.jpg)
Next steps
.png)

Supporting Adolescents’ SRH journeys every step of the way, one potli at a time







